EU regulators originally said no to Alzheimer's anti-amyloid mab drug Leqembi for European patients. Now, they've changed their minds.
In July 2024, European regulators rejected Eisai and Biogen’s anti-amyloid drug Leqembi for early stage Alzheimer’s. By November, they had changed their minds. Now, the drug is officially approved for certain patients living with early-stage Alzheimer’s disease in Europe — as long as they do not carry two copies of Alzheimer’s risk gene ApoE4.
Originally, the European Medicines Agency (Europe’s version of the U.S. Food and Drug Administration) said that the small impact the drug had on slowing cognitive decline did not outweigh its risk of the side effects of brain swelling and brain bleeding. Eisai requested regulators re-examine the data. And by November, the EMA had issued a new opinion — one that approves the drug for a more limited audience:
“After re-examining its initial opinion,” the November 2024 statement read, the regulatory committee approved Leqembi “for treating mild cognitive impairment (memory and thinking problems) or mild dementia due to Alzheimer’s disease (early Alzheimer’s disease) in patients who have only one or no copy of ApoE4, a certain form of the gene for the protein apolipoprotein E.”
Ultimately, regulators concluded, in these specific populations, “the benefits of Leqembi in slowing down progression of symptoms of the disease are greater than its risks.” The opinion was sent to the EU’s governing body, the European Commission, which this month finalized the decision to approve the drug.
Leqembi is approved in the UK under similar restrictions with a broader approval, which includes patients with two copies of ApoE4 in the U.S., Japan, China, South Korea, Hong Kong, Israel, and the UAE without restrictions. (Australia refused to grant the drug approval earlier this year.)
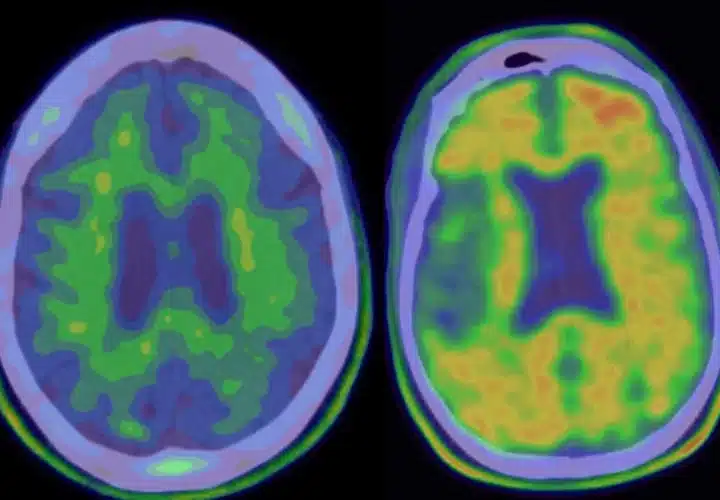
People with two copies of the ApoE4 gene have a higher risk of brain swelling and bleeds (ARIA). Clinicians have conflicting opinions about the drug’s safety and effectiveness overall.
Alzheimer’s Drugs and ARIA: Leqembi ‘Brain Bleeds’ Side Effect, Explained
The data behind the EMA’s revised opinion
European regulators checked to see whether leaving out patients with two copies of ApoE4 would substantially drop the ARIA rates.
Overall, one in eight trial participants developed brain swelling (ARIA-E) while about one in six developed brain bleeds (ARIA-H). But in the subpopulation with zero or one copy of ApoE4, the rates of ARIA-E dropped to one in 11 and ARIA-H to one in eight.
The Leqembi clinical trial measured the patient’s disease progression using a standardized 18-point dementia scale over 18 months.
Participants in the placebo group declined by a total of 1.66 points while participants who received the drug only declined by 1.21 points. The difference of 0.45 points amounts to a relative slowing of cognitive decline by 27 percent.
Based on this analysis, the regulators concluded that the drug’s benefits outweighed the risks in people with one or zero copies of ApoE4, leading to a small slowing of cognitive decline.
Now that the European Commission has approved the drug, Eisai will have extra responsibilities. It will need to carry out a safety study to further assess the risk of ARIA-E and ARIA-H and set up an EU-wide database to track side effects, the long-term impact of ARIA, and how well Leqembi slows progression over time.
Eisai has no such requirements in the U.S. Instead, the Alzheimer’s Association has sponsored a voluntary database called ALZ-NET to track similar information.
UPDATE April 18, 2025: This November 2024 article was updated with new information regarding the EU regulators’ confirmation of this decision.



Has the medical researchers found any information on what causes dementia? Since older people don’t remember as well as younger people, is there any reading information or books about this topic?